In June of 2020, the area known as Alabama’s Black Belt was hit hard by the Coronavirus.
Overcoming a History of Racism and Medical Abuse
Alabama’s Black Belt, originally named for its rich, dark soil, is a poverty-stricken area, especially outside its small towns, with African Americans making up the majority of its population. Focus groups across Alabama are meeting to address vaccine hesitancy among communities of color, particularly among African Americans and other races.
There are many reasons why African Americans don’t get vaccinated, but one, in particular, stands out: the Tuskegee Study of Untreated Syphilis. Between 1932 and 1972, the United States Public Health Service conducted a study on black males. The purpose of this study was to observe the natural history of untreated syphilis – the men were told they were getting treated for “bad blood” but were not treated at all.
For many Black residents, they struggle to overcome a historical mistrust of the government and the health system because of neglect and racist medical
abuse as shown in the decades-long, government-sponsored Tuskegee study. This example of malpractice is far from forgotten by the Black community.
Providing Accurate COVID-19 Information
There is also concern that many unvaccinated African Americans don’t oppose vaccination, but have trouble making the time to get vaccinated, or haven’t felt strongly motivated to do so.
Being transparent about information of the COVID-19 vaccination and Coronavirus, and all its factors play a major role in the Black communities, especially in this day and age. Having a reliable source and the right people to get the information out can be useful to the Black communities.
With only one COVID-19 vaccine, Pfizer, being fully approved by the FDA, the agency has granted emergency use authorization to two other COVID-19 vaccines used in the United States: Moderna and Johnson & Johnson.
Public Health Efforts Help Vaccine Rates
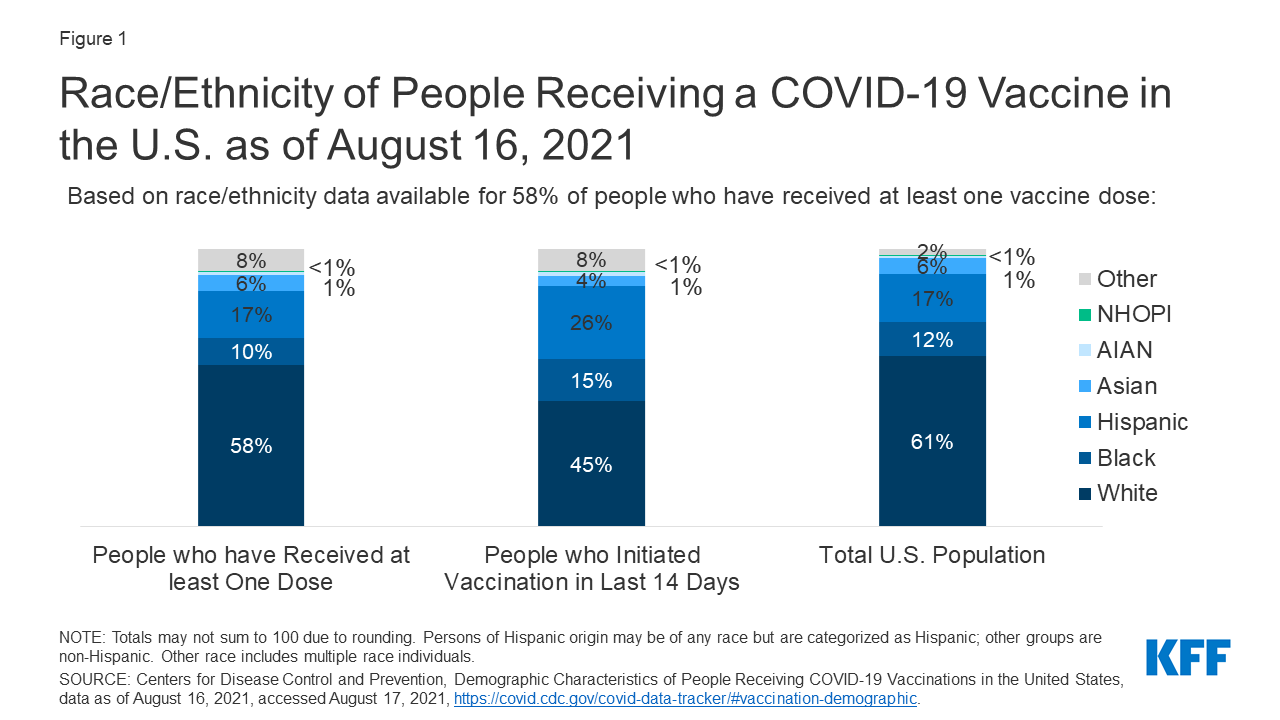
ADPH says the Black Belt region has the highest percentage of people getting COVID-19 vaccinations. Successful public health efforts to achieve vaccine equity have resulted in higher vaccine uptake among African American residents of Black Belt counties.
In this historic region of Black Belt counties, home to large populations of Black residents, some jurisdictions have completed vaccinations at rates of over 40%. Overall in Alabama, as of August 2021, about 34% of the population is fully vaccinated, according to the Centers for Disease Control and Prevention (CDC). Some counties in the Black Belt have more people fully vaccinated than the state as a whole, while some have a lower percentage.
Not only are we struggling with getting vaccination in Alabama, but surrounding states have the same issues.
Unvaccinated People Most at Risk for Delta Variant
With COVID-19 cases on the rise again, there is a big push to get more people vaccinated. COVID-19 cases are up mainly due to the high transmission of the Delta variant that is now spreading. Unvaccinated people are most at risk, but there have been some breakthrough COVID-19 cases among the vaccinated population.
Furthermore, the vast majority of hospitalizations and ICU cases are among unvaccinated people. The bottom line is that the COVID-19 vaccines are effective in preventing both infections and deaths.
Combating New COVID-19 Strains
The rise in COVID-19 cases is concerning because the disease is preventable. If more people got the vaccine, we would be much closer to full immunity, and there would not be a variant surge.
According to the CDC, approximately 99.4 percent of COVID-19 deaths in the United States are among unvaccinated people. Why are breakthrough infections less harmful? Studies have shown the vaccine not only protects against the virus that causes COVID-19 but also against new strains that are developing, including the Delta variant.
Immune Systems Can’t Fight COVID-19 Without a Vaccine
COVID-19 vaccinations have been largely voluntary, and many people have not gotten around to getting the vaccine for
one reason or another. Not getting vaccinated puts one at greater risk of severe illness if infected and also may cause death. When someone who is unvaccinated is exposed to the COVID-19 virus, protection from the virus comes from the body’s innate immune system or innate defenders, which are responsible for rapid, non-specific responses to pathogens and harmful substances.
COVID-19 is an evasive virus, and it can wreak havoc on the body before it can mount an adequate response. The adaptive immune system is responsible
for antigen-specific immune responses, but its initial response to an antigen can be slow.
An unvaccinated person’s immune system might eventually produce a stronger response to the virus, but that process could take weeks. By then, the
the virus may have caused a lot of harm and resulted in serious illness, long-term damage, or death.
View COVID-19 resources here.